The Surprising History of Anti-Vaxxers and Measles
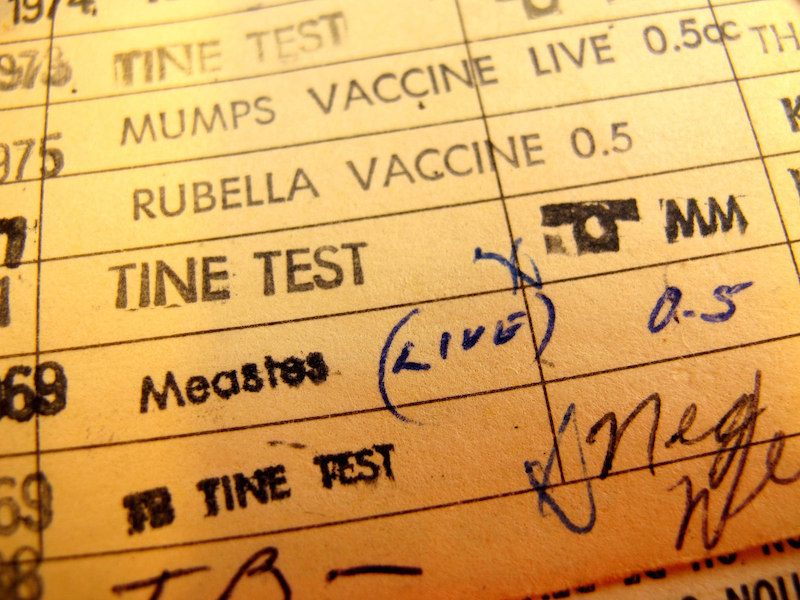
It took decades for most of the population to receive the measles vaccine. (Photo: frankieleon/Flickr)
In 1954, Thomas Peebles, a pediatrician, went to Boston with a mission: taking blood from young men with measles. One of the samples he collected came from a student named David Edmonston. Within a decade, the lab Peebles worked for, run by the Nobel Prize-winning virologist John Enders, had transformed that sample—the virus cultured from Edmonston’s blood—into the first measles vaccine.
Even in the earliest days of measles inoculation some parents were skeptical of the vaccine, though not for unfounded fears of autism. Before the 1960s, millions of people would contract measles every year, and hundreds, just in the U.S., would die. But yet measles wasn’t thought of as a particularly dangerous disease. Mostly, the vaccine just didn’t seem worth it to some people: why bother with the risk (and there was some), when most people got the measles, and most survived?
When it came time to vaccinate his own kids, even the vaccine’s source, Edmonston, chose not to.
But, besides sparing kids from itchy rashes and spots, the measles vaccine had an amazing and mysterious effect: The first mass measles vaccinations campaigns led to drops in childhood death so dramatic that they have never been entirely explained. One group of infectious disease experts, though, thinks they know what happened—and what they discovered makes the idea of skipping vaccinations seem even more dangerously backward.
In a new paper, published this week in Science, these researchers argue that measles infections essentially wipe out the immune system’s memory—immunity acquired earlier in life is cleared away. And so, after having measles, kids might get sick for years afterwards from diseases to which they were once resistant. The researchers show that, in the years before the vaccine was developed, measles infections were responsible, at least indirectly, for about half of all childhood deaths from infectious diseases.
“That raises eyebrows,” says Michael Mina, the paper’s lead author, an M.D.-Ph.D. studying infectious disease at Emory University. If measles was connected to so many deaths, why hadn’t anyone discovered that yet? “It’s not a direct effect,” Mina says. “A kid might get pneumonia two years after getting measles, and it’d just be attributed to bad luck.”
Mina and his colleagues looked at data from affluent countries—England, Wales, the US, and Denmark—where childhood mortality was relatively low, so that they could more clearly pinpoint any change in the death rate connected to the measles. And their results showed that, given measles’ connection to subsequent infections, they could account “for nearly all of the inter-annual fluctuations in childhood infectious disease deaths,” they report. In other words, even if it wasn’t clear that these kids were dying from the measles, the measles was still responsible for their deaths.
There was no way parents in the 1960s and ’70s could have known that, of course. Parents didn’t prioritize getting their kids vaccinated: likely they thought, like David Edmonston’s wife, that “in this country, measles isn’t that bad a thing,” as Arthur Allen reports in Vaccine. To get a sense of how casually people treated the disease, consider the Brady Bunch’s perspective: “If you have to get sick, sure can’t beat the measles.”
“Measles is such an interesting infection,” says Mina. “It was the number one cause of childhood death, before the vaccine was around. But it infects so many kids that, on a case-by-case basis, the risk of getting the worst effects was relatively low. It led people to not really think of measles as a terrible disease.”
But what his and his colleagues’ work shows is that, even beyond the deaths measles was directly responsible for, it functioned as a sort of shadowy assassin that left other diseases do its dirty work. And that makes today’s measles outbreaks—small by pre-vaccine standards, but some of the largest in recent U.S. history—even more alarming. If measles can delete already acquired immunities, as vaccination rates fall, the kids who are contracting this preventable disease are being put at higher risk for a slew of other dangerous diseases.
Mina’s own views on vaccination were shaped, in part, by growing up in communities where not everyone accepted them. “I was raised in a family that was open to both Western and alternative medicine,” he said. “I had this chiropractor, and he was totally against getting vaccines, and he ended up dying when I was 8 or 9 because he refused to use antibiotics and deal with Western medicine.” In high school, Mina went to a Waldorf school where many of his classmates were unvaccinated, and he says, “I was always yelling at my friends’ parents because they weren’t getting their kids vaccinated.” Later, after he had moved to Sri Lanka, he “ended up becoming a Buddhist monk for awhile” and landed, in the wake of the 2004 tsunami, in a refugee camp where infectious diseases were widespread, he decided to focus his career on studying them.
“Measles is far from a benign infection,” he says. “It has these large, long term consequences that put children at risk for other diseases. And I think it just drives home the message that we really need to be diligent about vaccinating our kids.”









Follow us on Twitter to get the latest on the world's hidden wonders.
Like us on Facebook to get the latest on the world's hidden wonders.
Follow us on Twitter Like us on Facebook