Do You Have The Guts To Watch VR Surgery?
Hanging out in an operating room hundreds of miles away.
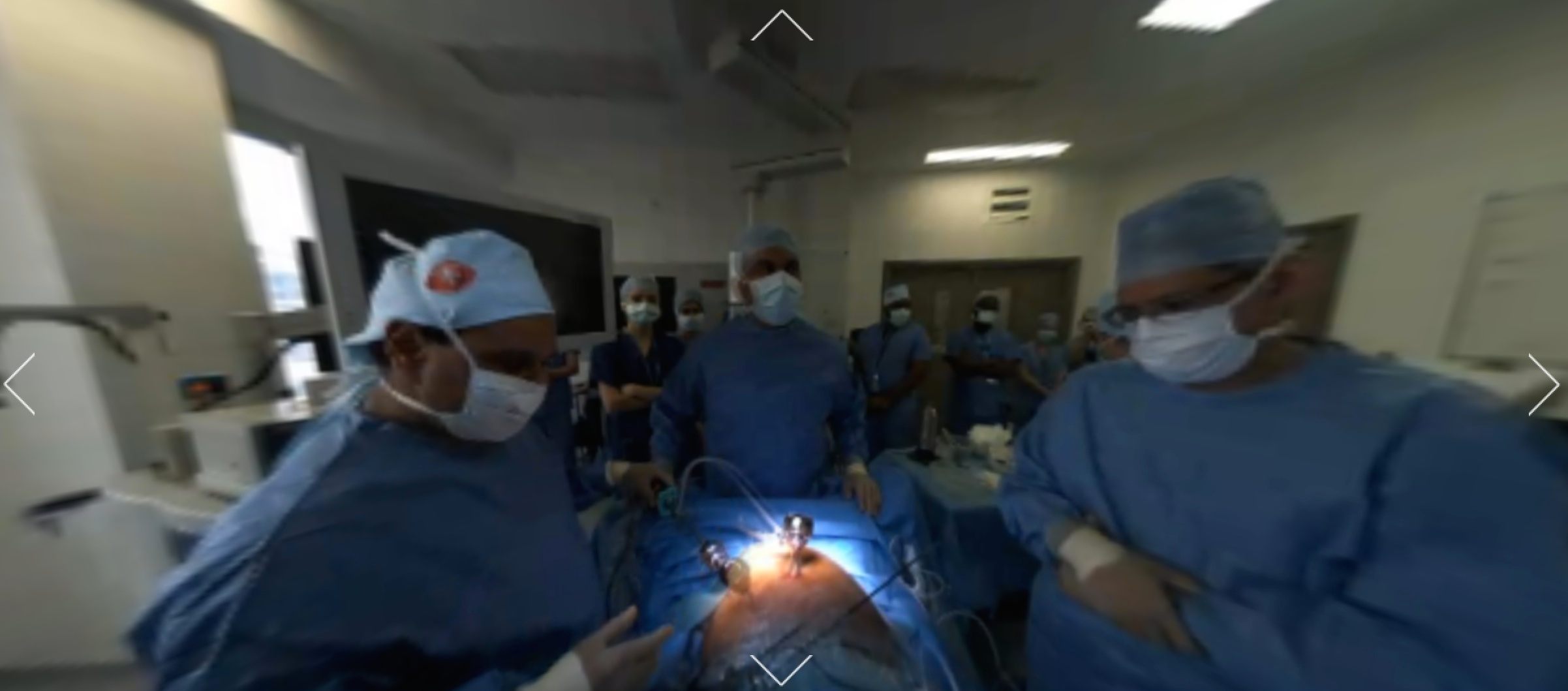
Scrubbing in… virtually. (Image: Medical Realities)

Yesterday morning I woke up, sat on my couch, set a $15 Google Cardboard on my nose—and “stood,” for two hours, in a London operating room, as a dozen doctors carved a tumor out of a patient’s colon.
This is not an intuitive way for me to start the day. If I ever end up in a real, physical operating room, I’ll likely be wheeled in on a gurney. When I texted a second-year med student friend that I was spending my morning virtually scrubbing into a tumorectomy, she replied immediately: “Get ready to be bored.” And for the next two hours, I got pretty bored—but I also got the inside scoop on the human body, grew soothed by the soft beeping of various machines, and kept tabs as a few dozen pairs of gloves got slowly bloodier. Along the way, I tapped into a couple of emotional currents I didn’t know I would ever be able to access.
This was the first surgery ever broadcast over an immersive VR platform, and I was far from alone in my desire to participate in this small biopsy of history. Classrooms full of med students strapped on headsets to watch. Former hospital workers took a jaunt down memory lane (“my moms at 69 who used to be a candy striper in the 60s is LOVING being back in an OR,” tweeted one fan).
Doctors posted pictures of their begoggled faces with notes of encouragement. “Thinking back to my time as a medical student and junior doctor, the only thing that was missing was an anesthetist quietly completing a the Telegraph crossword, while the lead surgeon screamed at me for not knowing the branches of the Mesenteric artery,” wrote Dr. Keith Grimes in an after-the-fact blog post. “Oh, and that smell.”
Amazed to have joined in with #VRinOR as part of our surgery module @QMULBartsTheLon @NHSBartsHealth @MedRealities pic.twitter.com/xj4ytVA99S
— Tom Cooke (@ThomasCooke) April 14, 2016
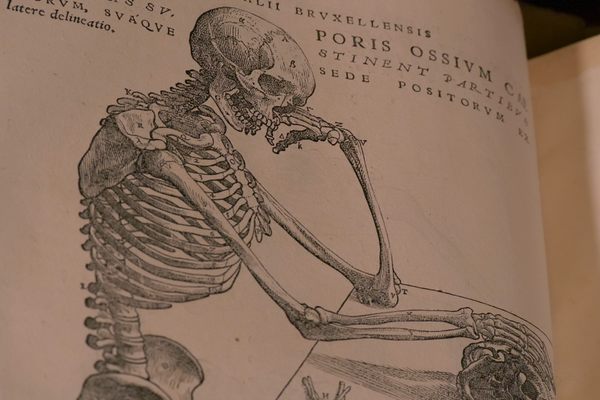
To put it in public broadcasting terms, this program was made possible by Dr. Shafi Ahmed, a 44-year-old surgeon and cancer specialist at The Royal London Hospital, and the co-founder of Medical Realities, a company that seeks to broaden the surgical training space by bringing in “virtual reality, augmented reality, and serious games.”
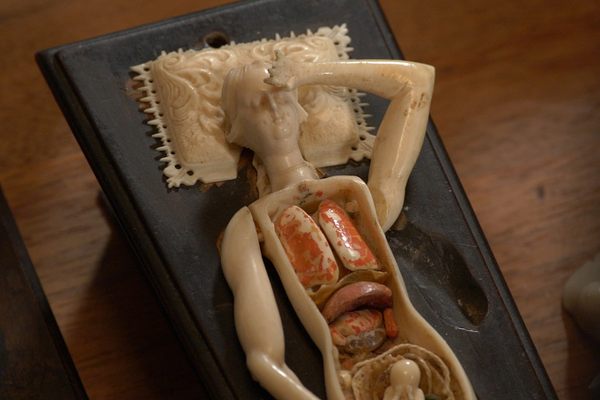
Ahmed thinks such immersive tools are the future of surgery, and has spent the past few years suturing these two areas of interest together. In 2014, he removed a liver tumor while wearing Google Glass, streaming the surgeon’s-eye-view experience live to 13,000 medical students, and answering their questions aloud as they popped up on his headset. Last year, his company began developing The Virtual Surgeon—a VR game that, he hopes, will eventually let players do the cutting themselves.
For now, the OR’s digital interlopers can only watch—an experience which, without Grey’s Anatomy-style soundtrack cues and camera angles, turns out to be surprisingly opaque. Doctors and nurses are covered nose-to-toes in almost-identical scrubs, and the gowned patient—in this case, a 70-year-old Londoner—becomes an anonymous square of whatever flesh requires intervention. There isn’t a lot for the less educated viewer to grasp onto.
Lacking these dramatic television standbys, I found myself relying on Ahmed as an emotional barometer. He started out downright jovial as he maneuvered the laproscope, talking about what everyone was seeing (“That’s the heart, just above the diaphragm… there’s the spleen!”) and the incredible fact that we were all seeing it.
“This will allow people on a very cheap scale to get access to teaching and training wherever they are,” he said, as he excised some scar tissue. I felt my own heart swell. One small snip for man, one giant (budget) cut for mankind.
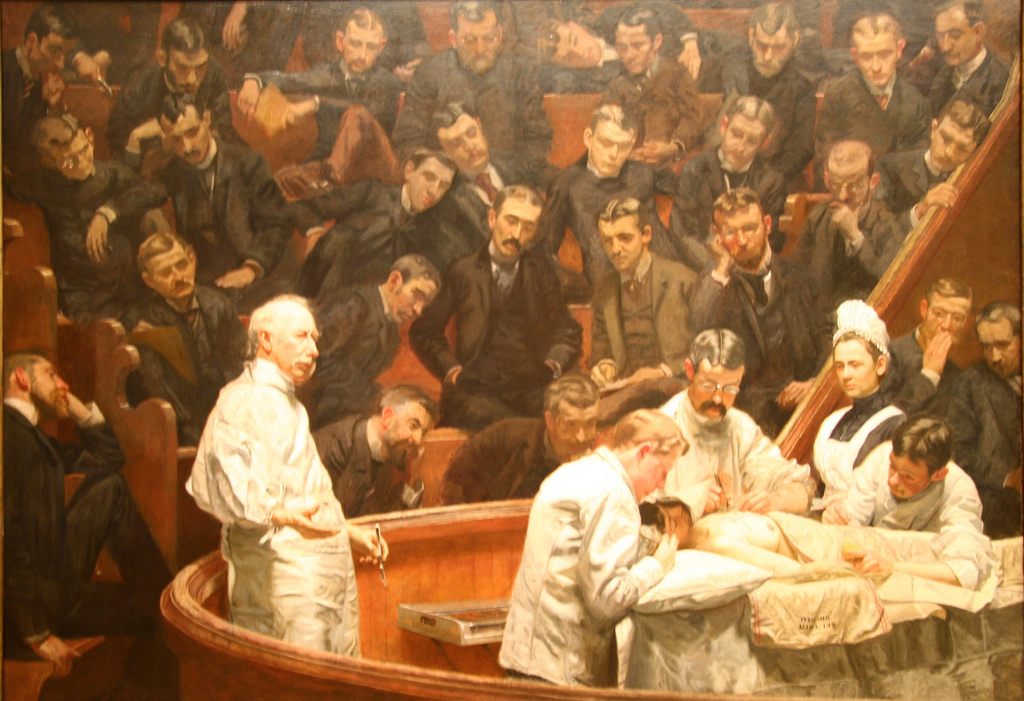
“The Agnew Clinic,” an 1889 oil painting by Thomas Eakin, shows a 19th century operating theater in action. (Image: Philadelphia Museum of Art/Public Domain)
Immersive, 360-degree livestreaming joins a long legacy of techniques designed to allow interested parties to witness the miracles of modern medicine up close. The early 1800s saw the separation of surgery from other hospital activities; soon after, surgeons began performing for rows upon rows of students and observers in operating theaters, designed less for patient hygiene or comfort than for the spectators’ efficient viewing.
In 1947, doctors at New York Hospital sent a live OR broadcast to the American College of Surgeon’s conference a few miles away. Surgery today already relies on screens—laproscopies, colonoscopies and other procedures depend on tiny cameras threaded through the bowels, and companies are working on enhancing the associated screens with IMAX-level definition and streaming the footage to educational theaters. Last October, National Geographic showed brain surgery on live TV for the first time, using both handheld and internal cameras.
On paper, going from a theater seat or a screening room to a set of goggles doesn’t sound like a big leap. In practice, though, it adds something like an extra sense. “I could choose to watch the anaesthetist if I wanted to, or the scrub nurse,” says Flora Malein, who watched the surgery along with the rest of her class at Barts and the London School of Medicine in Whitechapel. Someday, “we could have a 3-D camera attached to the scope in the bowel so that you could look around the inside of the bowel,” she predicts. “Now that would be something special!”
Half an hour into the surgery, looking for something special, I found myself “wandering” around the OR, seeing what I could see within the 360 available degrees. One minute, I was shoulder-to-shoulder with one of the surgeons, watching the slight shifts of his elbow as he maneuvered his long-handled scissors deep within the patient’s body. The next, I was zoomed in on the laproscopy screen, trying to figure out exactly where we “were” in the tissue. When I got squeamish, I turned my head and examine the shiny tools; when I got bored, I looked up at the skylight.

If you get bored, just go for weird angles. (Screenshot: Medical Realities)
At one point, Ahmed asked a trainee named Katherine to put on a headset and see how things were going for his wider audience. “It feels very real,” she reported. “It feels like I’m standing next to you.” (“Well, you are, really,” Ahmed responded.)
Because so many people can fit into a virtual room, such experiences also enable new conversations. Lydia Nicholas, an anthropologist who studies how medicine and technology interact, has watched a number of live surgeries in plain old 2-D, and says yesterday’s broadcast was an entirely different experience. “Livestreaming a surgery over my laptop… I know in my gut that it’s taking place far away,” she wrote in an email. “With the VR headset on, we are in the room.”
After passing some goggles around her office, she and her colleagues spoke about what they had seen as though they had been more than observers. ”It feels like a real experience,” she writes. “I think we all learned a little about the physical feeling of surgery—the expert’s technical skill of moving around, interacting between body, equipment and senses.”
VR proponents are hoping that, for medical students, this type of viewing experience might translate into increased skill with a real-life scalpel. For me, it was the opposite. About an hour into things, what had been a mostly bloodless jaunt through the digestive system via internal camera suddenly got gory. The doctors opened the patient up and began working directly with the tissue, pulling and snipping much more quickly than before.

Removing bloody gauze… in VR! (Screenshot: Medical Realities)
Ahmed stopped talking, save for the occasional clipped demand for implements, or for more light. The quiet, two-toned beeps of the machines sped up—or at least they seemed to. A friend who was also watching emailed me: “The doctors are stressed!” I suddenly felt the limits of my “presence” in the room. I was both doubly useless, and doubly aware of my uselessness—even if I had known how to help, I couldn’t have. I wasn’t really there.
But as things calmed down—and it became more clear that the situation was, and had been, under control—I began to see things in a different way. For those of us who aren’t doctors, being thrown into the middle of a surgery is the 21st-century version of bearing witness to a healing ritual—sometimes confusing, sometimes scary, and sometimes downright counterintuitive (isn’t anyone else nervous about all that blood?).
As Dr. Ahmed put in the final stitches, I felt both relieved and privileged. This strange confluence of blood and bloodlessness brings together medicine and space-and-time-shifting technology, two of the closest things to magic we’ve got. In the know or not, why wouldn’t we want to hang out in the middle?












Follow us on Twitter to get the latest on the world's hidden wonders.
Like us on Facebook to get the latest on the world's hidden wonders.
Follow us on Twitter Like us on Facebook